Weapon of Choice During Your RSI: PRE-OXYGENATION (2022 Update)
- Jared Patterson
- Nov 28, 2022
- 15 min read

In June of 2021, the first blog in this series was written regarding my “weapon of choice during RSI.” If you’re interested in catching up on this Deadpool theme I had, you can find the previous blog HERE. However, I am jumping straight to the point and removing the fluff this time, and covering pre-oxygenation. AGAIN — BUT WITH UPDATES!

I wanted the reader in my previous blog to choose a “weapon” that they thought to be the most important (typically an item from the above picture) to have on EVERY one of your future RSI’s and back up why you chose it. But, while writing the previous entry, instead of choosing an item for myself, I chose an approach from one of the 7 Ps of RSI. Pre-oxygenation was that weapon.

Now, when you look at the 7 Ps of RSI (pictured above and UPDATED), you may think to yourself, “Why are you choosing pre-oxygenation? Aren’t preparation, physiologic optimization, and all of the other Ps pretty damn important?” Yes, yes, they are. However, I tend to favor the physiologic side of RSI as it seems to be the least taught, more in-depth, and interesting subject (to me) regarding RSI. And… I like a little bit of disagreement with a highly educated rebuttal to opinions on this matter. Physiologic optimization would be a “same tier” choice for me, but putting them both into one blog would make for a much longer read than even I have the attention span for, and this is a LONG one.
The 7 Ps are one of many educational memory-aid tools used to teach RSI. Some of you may have heard of other mnemonics or the 8 Ps, but it’s all really the same 💩. Pre-oxygenation is one of those 7. Meaning that it is 1/7th of the entire procedure, roughly 14.285714% 😏. But I find it to be ONE of the most important. Why do you ask? Because of this:

^^^ This “Time to Hemoglobin Desaturation” chart, sometimes called the oxyhemoglobin desaturation curve, is the reason why I think pre-oxygenation is one of the most important “Ps” of the RSI procedure. The chart shows the time to desaturation in patients who have been adequately pre-oxygenated prior to induction. Look at it closely… study it… it’s actually pretty darned interesting and plays a large role in the rest of this blog.
Sidetrack #1: If you notice the box in the bottom right of the photo, you’ll also see that the patient’s oxygen percentages drop to critical levels before recovery from the administration of Succinylcholine. This chart does not eliminate any argument over the administration of Succinylcholine versus Rocuronium. If you are an “i WaNt ThEm tO sTaRt BrEaThInG aGaIn iF i mIsS tHe TuBe” pre-hospital provider, critical desaturation is often met before the return of spontaneous breathing. Also, in the paper “Rapid Sequence Induction and Intubation with Rocuronium-Sugammadex Compared with Succinylcholine: a Randomized Trial,” Rocuronium followed by the reversal with Sugammadex allowed for earlier re-establishment of spontaneous ventilation than with Succinylcholine [2]. I don’t know any EMS or pre-hospital service that carries Sugammadex, however, if you want them to breathe spontaneously sooner, maybe this should be a consideration 🤷♀️ . I think that if you chose to take that airway now, especially in the pre-hospital environment, in 10 minutes, the patient’s pathology likely hasn’t changed, and they will still require some sort of invasive airway… extra/supraglottic devices, anyone?

Alright, back from the side track…
Why is Pre-Ox Important?
Prevention of hypoxemia during airway management — that’s why! Not only is hypoxemia a terrifying complication, but it is associated with dysrhythmias, hemodynamic decompensation, hypoxic brain injury, and cardiac arrest [1, 3]. Hypoxemia could be avoided in many cases by meticulous pre-oxygenation, and with optimal pre-oxygenation, we can prolong the safe apnea time. Pre-oxygenation also creates an oxygen reservoir to be utilized by the patient while they are not breathing during the intubation procedure. Apnea is acceptable, provided the patient maintains normal oxygen saturation [1].
I believe we are doing our patient’s a disservice by not appropriately pre-oxygenating them before induction and paralysis. In my opinion, there is almost no reason ever not to make an attempt at pre-oxygenation prior to induction, and I'm sure many of you RSI nerds out there would agree with me 🤓. By appropriately pre-oxygenating our patients, we are making attempts to give them the best neurological outcome possible -- mitigating the effects of hypoxia during the procedure.
Now, I completely understand that we sometimes have no way of accurately estimating how long the patient will maintain oxygen saturation above the critical desaturation level. But what we do know is that we can prolong the safe apnea phase by making every effort we can to pre-oxygenate our patient.
I think Scott Weingart and Rich Levitan say it best in their paper, Pre-oxygenation and Prevention of Desaturation During Emergency Airway Management. They say, “It is impossible to predict the exact duration of safe apnea in a patient. Patients with high saturation levels on room air or after oxygen administration are at lower risk and may maintain adequate oxygen saturations as long as 8 minutes.”

What is Pre-Oxygenation?
Pre-oxygenation, per the Manual of Emergency Airway Management, is “The establishment of an oxygen reservoir within the lungs, blood, and body tissue to permit potentially several minutes of apnea to occur without clinically significant arterial desaturation.” With the administration of high-flow oxygen for 3 minutes, oxygen replaces the predominantly nitrogenous mixture of room air with oxygen, allowing several minutes of apnea time before hemoglobin saturation decreases to < 90%. If we adequately pre-oxygenate our patients, we buy ourselves time to complete the intubation procedure un-rushed and hopefully with a prolonged safe apnea time. Feeling “rushed” and becoming frantically nervous can make what was likely a routine intervention very complicated. I always use a quote while teaching this concept that I got from my older brother when he’d whoop my ass in video games: “Haste makes waste.”

This info always seems to potentially lead to the question:
What is Safe Apnea Time?
Safe apnea time is the time from the onset of apnea from induction until the patient experiences an oxygen saturation below 90% [1]. And as stated above, apnea is acceptable, provided the patient maintains a normal oxygen saturation. Safe apnea time can vary from several seconds to several minutes and is seen in the “Time to Desaturation” chart/picture [1]. The functional goal of pre-oxygenation, as well as apneic oxygenation, is to prolong the safe apnea time (or duration of apnea without desaturation [DAWD]) [3].
The time to desaturation to 90%, the safe apnea time, or DAWD, varies from individual to individual. Children, morbidly obese, chronic pulmonary disease, critical illness, and late-term pregnancy patients desaturate far more rapidly than the average healthy adult [1]. When you evaluate the “Time to Desaturation” chart, you notice that a patient maintains an appropriate oxygen saturation, if adequately pre-oxygenated, for several minutes. But, once approximately 90% is met, a precipitous drop from 89% to DEATH% occurs. This approximation at around 90% is what I have heard some refer to as the critical desaturation range.

What's App...neic Oxygenation?
Apneic oxygenation, or “Ap-Ox” as some call it, is just as simple as the word implies: Oxygenation occurring while the patient ceases to breathe (AKA apnea). 😱 😜

Apneic oxygenation is typically applied by a standard nasal cannula with flow rates between 5 and 15 LPM. Because oxygen diffuses across the alveoli more readily than carbon dioxide and has a high affinity for hemoglobin, more oxygen leaves the alveoli than carbon dioxide enters during apnea. This creates a gradient that causes oxygen to travel from the nasopharynx to the alveoli and into the bloodstream by a physiologic principle known as “aventilatory mass flow” [1]. I think of aventilatory mass flow as a vacuum, if you will, pulling the gases from above (which is the naso/oropharynx) down and into the alveoli. As long as the “gas” being pulled down is oxygen, our patients can be effectively oxygenated without breathing or receiving any manual ventilation.
You can read more on this in another of my previous blogs, “What’s App…neic Oxygenation,” HERE.
Per the Manual of Emergency Airway Management textbook, a standard nasal cannula is placed beneath the main pre-oxygenation device and is to be left in place for the duration of the intubation.
The Awake Patient:
Standard NC flow rate as high as the patient can tolerate, typically between 5 and 15 LPM.
The Comatose/Unresponsive Patient:
Standard NC set to at least 15 LPM.
During the Intubation Attempt (Sedated and Paralyzed):
The NC should be set to at least 15 LPM.
If nasal obstruction is present, a nasopharyngeal airway can be placed in both nares to facilitate oxygen delivery.
The patient should be ideally positioned for intubation, and a jaw thrust maneuver should be performed to ensure upper airway patency.
Sidetrack #2: If you are concerned about pH or EtCO2 during the apneic phase of the RSI, this paper by West, et al. (2017) may interest you. It’s titled “The Effect of the Apneic Period on the Respiratory Physiology of Patients Undergoing Intubation in the Emergency Department.” It showed that an apneic phase of greater than 60 seconds caused statistically significant changes in pH and PaCO2 by 0.15 and 12.5, respectively [4]. Another read of interest from a VERY OLD paper published in Anesthesiology in 1961 titled, “The Rate of Rise of PaCO2 in the Apneic Anesthetized Patient,” reported CO2 rise within the first minute of apnea between 8 and 16 mmHg with a subsequent and linear rise of 3.0 mmHg per minute following [5]. While old, I have seen the paper cited in many online readings while preparing for this blog. I don’t believe these papers offer answers to the specific question you may have (and so did I), which is: “Will apnea leading to a lowered pH and increased EtCO2 kill my patient?” That’s not for me to answer. However, having an idea of an approximate change in those values may lead you to believe harm could come from it. If the pH were 7.0 when you started the intubation procedure, I would have a strong index of suspicion that if it takes longer than a minute to intubate the patient during the apnea phase, the values could drop to critical, life-threatening levels. Many resources available recommend bagging the patient during the apnea time in an attempt to prevent any further drop in pH in patients who may be at risk.
How Do I Pre-Ox My Patient?
Ah, finally, the climax of the blog! And it’s pretty simple… kinda. And there’s still a ton to cover. 😬😬😬
You deliver 100% oxygen for 3 - 5 minutes to your patient by whatever method is appropriate for the patient’s condition. Alternatively, cooperative patients with healthy lungs can be pre-oxygenated by having them perform eight maximal volume deep breaths while breathing 100% oxygen [1]. The goal is to deliver the highest FiO2 possible in order to establish a reservoir of oxygen within the lungs - replacing mixed alveolar gases, such as the predominant nitrogen - with oxygen. This creates an oxygen reserve which will provide a source of oxygen the pulmonary circulation can still utilize during the apneic period prior to the insertion of an airway device.
The answer really is that simple: Administer 100% oxygen for 3-5 minutes by whatever method appropriate. If you do just that, you will have effectively pre-oxygenated your patient. But I’m also beating around the bush. Because the better question is: “How SPECIFICALLY do I administer 100% oxygen for 3-5 minutes by whatever method is appropriate?”

I’ll get to that, but first… a tidbit of what I think is necessary education PEARLS, if you will, that will help with understanding the method to pre-oxygenating our patients, because the method does seem a tad out of the ordinary.
PEARL #1
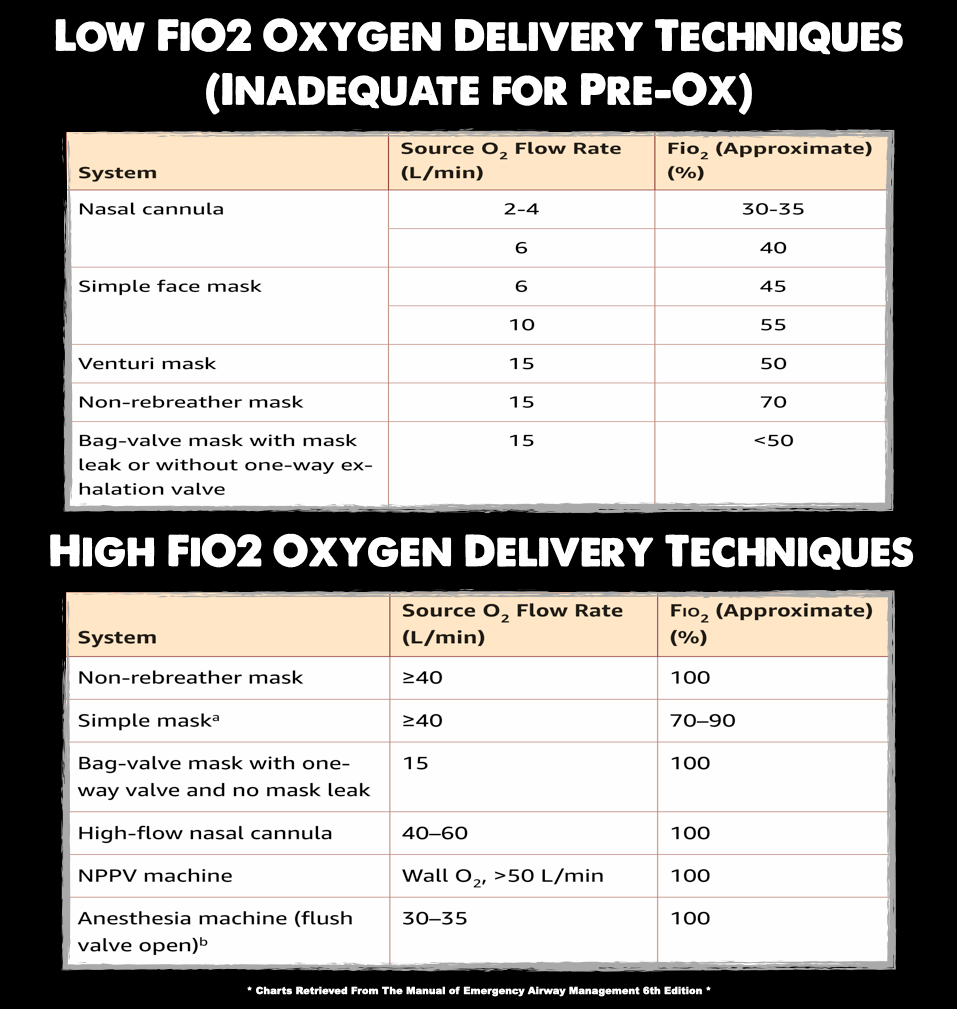
Traditional supplemental oxygen delivery devices are deceiving. I bet you’ve been led to believe that the non-rebreather mask (NRB/NRM) you have in the ambulance or emergency room is capable of delivering 100% oxygen. I was under that impression as well — paramedic school taught it to me, and it says so in some of the books. And it’s true, you can actually deliver 100% oxygen if you have an actual non-rebreather mask with two functioning one-way valves, a full reservoir bag, and a perfect mask seal… Oh, and with a liter flow exceeding the patient’s current minute ventilation.
But I bet that if you pulled out that non-rebreather mask from your department's stock, it only has one, one-way valve and another opening on the other side of the mask that is open to the atmosphere. Getting a perfect seal on that deformed piece of plastic? Good luck! And I bet you set the oxygen to an insufficient 10 - 15 LPM on the mask too… This all allows for the possible entrainment of room air through the device if the patient has a high minute volume while sucking wind prior to your RSI procedure. This means that your device is likely limited to, at best, 70% FiO2 delivery [1]. Which, we want as close to 100% as possible when pre-oxygenating our patients for RSI. Remember… 3 to 5 minutes of 100% oxygen.

This entrainment of room air ruining your delivery of 100% oxygen can be mitigated by altering our standard flow rates. If we set our flow meters to “flush” rates (> 40 LPM), it is possible to approach an FiO2 delivery of 100% [1]. This is usually only possible if you have a Thorpe Tube available. Traditional flow meters on portable oxygen devices seen in the pre-hospital environment usually allow for a max flow of 15 to 25 LPM.

For a more in-depth dive into this logic, read Sam Ireland’s blog: You Versus the Atmosphere (100% FiO2).
PEARL #2
You may be caring for patients in the pre-hospital environment and are working with devices that have limited liter flow, oftentimes restricted to 15 LPM (or 25 LPM in some). This makes the previous PEARL difficult to accomplish. How are you supposed to apply “flush” rate oxygen to your patients?
That’s where the nasal cannula comes into play. Not only is it a commonly accepted adjunct to pre-oxygenation [6], but it can be utilized for apneic oxygenation as well. You simply apply the nasal cannula under the non-rebreather mask and run the nasal cannula at the highest flow the patient can tolerate. This would effectively deliver approximately 30 to 50 LPM of oxygen during your pre-ox in conjunction with the non-rebreather (with BOTH set to the highest flow possible; if you can increase the NC or NRB flow higher, do it — MAX FLOW, BABY!!)
The pitfalls to this are needing two oxygen cylinders capable of delivering the required flow and your overall supply of oxygen — running oxygen at these liter flows will deplete the already limited oxygen supply for pre-hospital providers. In situations where oxygen supplies are limited, it is prudent to use just enough oxygen to maintain the desired level of oxygenation [1].
DO NOT USE THE EtCO2 NASAL CANNULA FOR PRE-OXYGENATION

EtCO2 nasal cannulas, or capno-lines as some call them, don't deliver oxygen through the nasal prongs as a standard cannula does. Oftentimes, in the EtCO2 variation, those prongs are used for aspiration of exhaled gases for your cardiac monitor to give you that qualitative and quantitative CO2 reading. It is your responsibility to know your department's equipment and understand how the device works.
PEARL #3
The BVM is capable of delivering 100% FiO2 at 15 LPM with a robust mask seal maintained. This can be utilized for your apneic and spontaneously breathing patients [1]. But keep in mind, if the seal is broken or inadequate, the patient may draw in room air around the mask during inspiration which could lower the FiO2 delivered substantially [1].
One should also be acutely aware that not all BVMs are the same. A bag-valve mask WITHOUT a one-way exhalation valve allows room air into the mix. A bag-valve mask WITH a one-way exhalation valve is capable of providing 100% oxygen, again only if a perfect mask seal is maintained.
A BVM is primarily reserved for patients who require active bagging either in between intubation attempts during the RSI or in the pre-intubation period when significant hypopnea manifests [1].
Although squeezing the bag in synchrony with patient inspiration is commonly performed for preoxygenation and is believed to augment oxygen delivery to spontaneously breathing patients, this practice should be avoided. Squeezing the bag in near synchrony is technically difficult, provides minimal positive pressure, requires additional attention paid to the patient’s respiratory cycle, and performs similarly to creating a tight mask seal without bagging. If a spontaneously breathing patient truly needs positive pressure ventilation for oxygenation, a noninvasive positive pressure machine should be used when time permits [1].
I will direct you to another one of Sam Ireland's blogs: The FiO2 Fallacy, where Sam, this time, dives into the anatomy of a BVM. I highly suggest you read it!
PEARL #4
Non-invasive positive pressure ventilation; NIPPV, or CPAP/BiPAP for those 👏 you 👏 in 👏 back (Sorry, I had to use the clap out of sarcasm... I hate when I see it, especially with that sentence 😏 ). Late-term pregnancy, morbidly obese, or patients with shunt physiology, such as pulmonary edema, severe pneumonia, or ARDS, may require NIPPV. These patients have alveoli that may be perfused, but not ventilated, requiring increased airway pressure to open the alveoli for maximal oxygen storage and optimal gas exchange. NIPPV provides that pressure.
Patients who remain hypoxemic (SpO2 <93%) despite maximal attempts at pre-oxygenation and those with compressive atelectasis (late-term pregnancy, morbidly obese, severe ascites) NEED positive pressure ventilation.
PEARL #5
Position your patient upright, if possible. Oxygen storing capacity within the lungs is the greatest when the patients are sitting up. Pre-oxygenation is significantly more effective when the patient is upright, allowing better use of the patient’s functional residual capacity (FRC; the area the blood will draw oxygen from during the apneic phase).
Even if you are ventilating an apneic patient with a bag-valve mask, head elevation at 20 to 30 degrees is better than supine.
PEARL #6
When we are pre-oxygenating our patients, we are also hoping that they become denitrogenated as well — that’s part of the 3-5 minutes we spend with the patient on “flush” rate oxygen flow.
As you sit currently, you are inhaling approximately 21% oxygen, 78% nitrogen, and a fraction of other gases like farts. If we replace the predominant gas, nitrogen, within our lungs with oxygen, we are prolonging the safe apnea time.

** Sam's illustration used in his blog, You Versus the Atmosphere (100% FiO2). It demonstrates that 100% FiO2 is necessary to effectively "denitrogenate" our lungs 🫁 **
Ok, OK, OKAY!
I will now share with you, "How to specifically administer 100% oxygen to our patients."
The Pre-Oxygenation Procedure:
If the patient is spontaneously breathing with adequate respiratory drive, ensure airway patency and place them in an upright position. Then apply the following:
A standard nasal cannula (NOT the EtCO2 variant) prior to placement of the pre-oxygenation device for apneic oxygenation (also serves as a pre-oxygenation adjunct).
Set NC @ 5 to 15 LPM (as high as the patient will tolerate).
NC will remain in place and running until the ETT is placed.
Non-rebreather mask (yes, over the NC).
Set NRB at the highest LPM available
“Flush” rates are ideal (> 40 LPM).
If 15 LPM is as high as it goes, do it.
A patient who remains hypoxic (oxygen saturations < 93%), despite maximal passive oxygen delivery, is assumed to have shunt physiology, typically. This patient often requires NIPPV (CPAP or BiPAP). It is likely that PEEP is required to obtain appropriate oxygen saturation. This applies to obese and late-term pregnancy patients as well. Pre-oxygenate these patients as follows:
CPAP or BiPAP; set at parameters per patient care guidelines or protocols.
Typically, PEEP is started at 5 cmH20
Titrate up, as guidelines indicate
Nasal cannula in place as stated above.
It is possible to maintain a mask seal, most times, with a NC in place.
IF the patient has inadequate respiratory drive, is in need of some manual ventilation support, or apneic, utilize:
Bag-valve mask with a PEEP valve.
@ 15 LPM, or more
Ensure adequate mask seal
Give only gentle breaths
Reduces risk of emesis and aspiration
Do this for 3-5 minutes and get that oxygen saturation to 100%, ideally (or as high as possible). This should give you a “buffer” for the patient’s safety, prolonging the safe apnea time and mitigating the harmful effects of hypoxia.
If the oxygen saturation decreases to 93% or lower, or after intubation fails, the intubation attempt should be abandoned, and efforts should then focus on re-oxygenation/rescue oxygenation. High-quality bag-mask ventilation with a well-fitting mask must be provided and measured by:
Chest rise and fall
Auscultation
Waveform capnography (the same EtCO2 used for intubated patients, and yes, it works great)
The current BVM procedure recommended is with the “two thumbs up, two provider technique.”
If you are a part of an EMS/pre-hospital system with limited oxygen supplies or only one source of O2, consider the following:
Pre-oxygenating the patient with the NRB or BVM as described above, still with a NC below the currently flowing pre-oxygenation device of choice (not attached to oxygen, but in a place where it can soon be used).
Once the pre-oxygenation device of choice is removed or discontinued for the intubation attempt, apply that oxygen source to the NC for apneic oxygenation.
Conclusion
In my opinion, and I'm sure many others agree, you should do everything you can to increase the patient's oxygen saturation prior to inducing apnea. Deliver 100% oxygen, to the best of your ability, to your patient. By doing so, you are decreasing the patient's risk of dysrhythmia, hemodynamic instability, hypoxic brain injury, and just plain old death. If you have made every attempt to increase the patient's oxygen saturation and they still aren't increasing to what we all would call acceptable, move on with your procedure; consider inserting a supraglottic airway, continue ventilating with the bag-valve mask, or go to the knife (following your organization's guidelines of course 😏). If an adverse event is to occur due to hypoxia, we can at least tell ourselves that we took every precaution to reduce the likelihood of this outcome.
I know there is so much more to RSI than pre-oxygenation. But pre-oxygenation is one of those topics that I am not only passionate about, but I feel has saved my @$$ on multiple occasions. I'm not gonna knock the other "P's," but I will share that, in my opinion, pre-oxygenation is pretty darned important and would be my "Weapon of Choice" if you made me choose which part I thought was most crucial.
I know we all have our convictions when it comes to RSI. Which weapon or approach would you choose? Do you agree? Disagree?
Look out for a similar blog on physiologic optimization coming soon! Also, I may add "adjunct" blogs in the future regarding the use of HFNC for pre-oxygenation and apneic oxygenation, as well as something on EtO2 😜
BOOM! 💥
Jared Patterson, CCP-C, One Rad Medic
Killin' It Since 1989

Twitter: @OneRadMedic
Insta: OneRadMedic
1. Brown, C.A. and Walls, R.M. (2023) The Walls Manual of Emergency Airway Management. 6th edn. Edited by J.C. Sackles et al. Philadelphia, PA: Wolters Kluwer.
2. Sørensen MK, Bretlau C, Gätke MR, Sørensen AM, Rasmussen LS. Rapid sequence induction and intubation with rocuronium-sugammadex compared with succinylcholine: a randomized trial. Br J Anaesth. 2012 Apr;108(4):682-9. doi: 10.1093/bja/aer503. Epub 2012 Feb 6. PMID: 22315329.
3. Hagberg, C. (2022) Preoxygenation and Apneic Oxygenation for Airway Management for Anesthesia, UpToDate. Edited by S. Jones and M. Crowley. Available at: https://www.uptodate.com/contents/preoxygenation-and-apneic-oxygenation-for-airway-management-for-anesthesia#! (Accessed: November 23, 2022).
4. West JR, Scoccimarro A, Kramer C, Caputo ND. The effect of the apneic period on the respiratory physiology of patients undergoing intubation in the ED. Am J Emerg Med. 2017 Sep;35(9):1320-1323. doi: 10.1016/j.ajem.2017.03.076. Epub 2017 Apr 2. PMID: 28412161.
5. Eger EI, Severinghaus JW. The rate of rise of PaCO2 in the apneicanesthetized patient. Anesthesiology 1961;22:419–25.
6. Nickson, C. (2021) Preoxygenation, Life in the Fast Lane • LITFL. Available at: https://litfl.com/preoxygenation/ (Accessed: November 23, 2022).
7. Brown, C.A. and Sackles, J.C. (2020) Rapid Sequence Intubation for Adults Outside the Operating Room, UpToDate. Edited by R.M. Walls and J. Grayzel. Available at: https://www.uptodate.com/contents/rapid-sequence-intubation-for-adults-outside-the-operating-room?search=preoxygenation-and-apneic-oxygenation-&source=search_result&selectedTitle=10~67&usage_type=default&display_rank=10#H7 (Accessed: November 23, 2022).





Jared, nice write up. It might have just been easier to suggest to folks to take the Difficult Airway Course which covers all of this and then some, although I was happy to see you credited the reference book used for the course. Some of your graphics certainly are a little better then the ones we use when instructing the course and I perhaps we can find a way for them to incorporate.